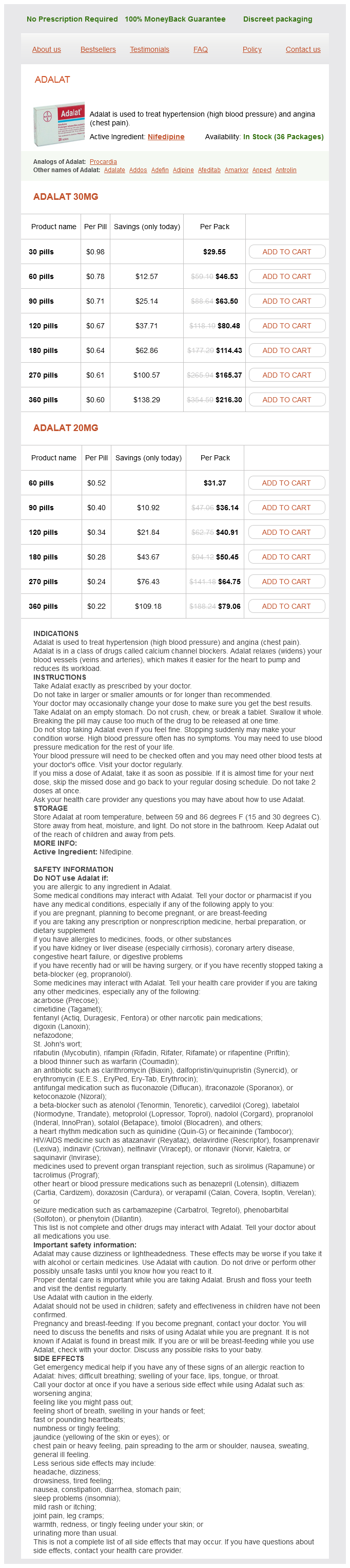
Adalat Dosage and Price
Adalat 30mg
- 30 pills - $29.55
- 60 pills - $46.53
- 90 pills - $63.50
- 120 pills - $80.48
- 180 pills - $114.43
- 270 pills - $165.37
- 360 pills - $216.30
Adalat 20mg
- 60 pills - $31.37
- 90 pills - $36.14
- 120 pills - $40.91
- 180 pills - $50.45
- 270 pills - $64.75
- 360 pills - $79.06
In the case of epidermolysis bullosapyloric atresiaobstructive uropathy association pulse pressure variation purchase 30 mg adalat fast delivery, mutations in the 6 and 4 integrin subunits of the hemidesmosome have been noted. Newborn infants with any variant of gastric atresia have signs of gastric outlet obstruction including onset of forceful, nonbilious emesis following the first feeding. When diagnosis is delayed, severe metabolic alkalosis, volume depletion, and shock occur; prolonged gastric distention may result in gastric perforation. Abdominal radiographs demonstrate gaseous distention of the stomach and a gasless intestine. These lesions, except for the presence of membrane perforations, are identical to the membranes of gastric atresia. Luminal narrowing is from the malformation itself as well as from local inflammation and edema. The primary symptom is vomiting, which in infants or children may result in failure to establish normal weight gain. In older children and adults, the symptoms may mimic those of peptic ulcer disease, with nausea, epigastric pain, and weight loss. The abdominal radiograph is typically normal, although gastric distention may be noted. Contrast radiography demonstrates the membrane as a thin, circumferential filling defect in the antrum or pylorus. Careful observation shows contrast material with delayed passage through a central defect in the membrane; overall gastric emptying is delayed. Clinical Features and Diagnosis the infant typically presents with postprandial vomiting and malnutrition. There may also be diarrhea (a result of rapid gastric emptying) and dumping syndrome. Respiratory symptoms, including respiratory distress at birth and stridor, as well as recurrent pulmonary infections, have been reported. Anemia due to iron deficiency may occur because decreased gastric acid secretion may preclude adequate iron absorption; cobalamin (vitamin B12) deficiency may follow hyposecretion of intrinsic factor. The lower esophageal sphincter is poorly defined, and esophagogastric reflux is usually severe. Treatment the medical management of microgastria includes frequent small-volume feedings or continuous-drip feedings into the stomach. An alternative is nocturnal drip feedings via jejunostomy to supplement oral intake. The surgical creation of a double-lumen Roux-en-Y pouch anastomosed to the greater curvature of the stomach has been described. This Hunt-Lawrence jejunal pouch has allowed normal growth and development and prevented reflux and dumping syndrome. The presence of a concomitant duodenal atresia has been described (also known as windsock diaphragm [see Chapter 25]), and its presence or absence is verified by passage of a catheter distally into the duodenum intraoperatively. Endoscopic therapy using a snare, papillotome, laser, or dilation via balloon also has been described. An alternative approach is pyloric sphincter reconstruction via longitudinal pyloromyotomy, followed by end-to-end anastomosis of culde-sacs of gastric and duodenal mucosa. The true congenital diverticulum contains all gastric tissue layers and is located on the posterior wall of the cardia. The intramural (or partial) diverticulum projects into but not through the muscular layer, most commonly located along the greater curvature of the antrum. The false (or pseudo-) diverticulum is formed by mucosal and submucosal herniation through a defect in the muscular wall and lacks muscularis propria. Clinical Features and Diagnosis Most congenital gastric diverticula are asymptomatic and are incidental findings on radiography or endoscopy, or at autopsy (see Chapter 25). Contrast radiography shows a rounded, well-delineated mobile pouch, often with an air-fluid level. On endoscopy, the diverticulum is seen as a well-delineated opening; distention by the scope may reproduce symptoms. Symptoms may be epigastric or lower chest pain, indigestion, bleeding, or nonbilious emesis. The differential diagnosis includes an acquired gastric diverticulum found in association with pancreatitis, gastric outlet obstruction, trauma, ulcer disease, or malignancy. Hiatal hernia and hypertrophic gastric folds may mimic a diverticulum on contrast studies. Microgastria Microgastria is an extremely rare congenital anomaly of the caudal part of the foregut. A small, tubular or saccular, incompletely rotated stomach is associated with a megaesophagus. Varying degrees of the anomaly occur owing to arrested development during the fifth week of gestation in differentiation of the greater curvature of the stomach such that neither rotation nor fusiform dilation of the stomach occurs. Microgastria may occur as an isolated anomaly but more commonly in association with other anomalies: duodenal atresia; nonrotation of the midgut; ileal duplication; hiatal hernia; asplenia; partial situs inversus; or renal, upper limb (microgastria limb reduction anomaly), cardiac, pulmonary, skeletal, or spinal. It has been suggested that microgastria in association with limb reduction defects and central nervous system anomalies has a genetic basis, with an autosomal recessive pattern of inheritance. Treatment In the case of an incidentally discovered proximal gastric diverticulum, treatment is unnecessary. Because of the risk of malignancy associated with distal gastric diverticula, surgical treatment by amputation, invagination, or segmental resection has been recommended. Aside from concurrent duplications, vertebral anomalies are the second most commonly linked abnormality. Location is contiguous with the stomach, generally along the greater curvature or posterior wall, and contains all layers of the gastric wall. Infrequently there may be a connection to the colon, pancreas, or pancreatic duplication; the connection may be the result of an acquired fistula from a penetrating peptic ulcer within the gastric duplication.
Dysphagia was frequent heart attack kid adalat 20 mg buy fast delivery, occurring in 68% of patients postoperatively, 11% at 1 year, and 4% at 3 years. Randomised clinical trial: High-dose acid suppression for chronic cough-A double-blind, placebo-controlled study. American Gastroenterological Association technical review on the management of gastroesophageal reflux disease. Esophageal pH-impedance monitoring in patients with therapy resistant reflux systems: "On" or "off" proton pump inhibitors Value of preoperative esophageal function studies before laparoscopic antireflux surgery. Prevalence and clinical spectrum of gastroesophageal reflux: A population-based study in Olmsted County, Minnesota. Prevalence, knowledge and care patterns for gastro-oesophageal reflux disease in United States minority populations. Gastro-oesophageal reflux symptoms and health-related quality of life in the adult general population-The Kalixanda study. Gastroesophageal reflux disease symptoms: Prevalence, sociodemographics and treatment patterns in the adult Israeli population. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: Report of the Indian Society of Gastroenterology Task Force. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: A national population-based study. Body mass index, chronic atrophic gastritis and heartburn: A population-based study among 8936 older adults from Germany. Helicobacter pylori and gastroesophageal reflux disease: the bug may not be all bad. Risk of gastrointestinal malignancies and mechanisms of cancer development with obesity and its treatment. Association between body mass and adenocarcinoma of the esophagus and gastric cardia. Increasing insulin resistance is associated with increased severity and prevalence of gastro-oesophageal reflux disease. Are lifestyle measures effective in patients with gastroesophageal reflux disease Endoscopic findings in patients presenting with dysphagia: Analysis of a national endoscopy database. Comparison of prescription drug costs in the United States and the United Kingdom, part 2: Proton pump inhibitors. Burden of gastro-oesophageal reflux disease in patients with persistent and intense symptoms despite proton pump inhibitor therapy: A post hoc analysis of the 2007 national health and wellness survey. Systematic review: the association between symptomatic response to proton pump inhibitors and health-related quality of life in patients with gastrooesophageal reflux disease. Determinants of gastroesophageal junction incompetence: Hiatal hernia, lower esophageal sphincter, or both Electrical and mechanical activity in the human lower esophageal sphincter during diaphragmatic contraction. Flow across the gastro-esophageal junction: Lessons from the sleeve sensor on the nature of anti-reflux barrier. Objective definition and detection of transient lower esophageal sphincter relaxation revisited: Is there room for improvement Mechanisms of lower esophageal sphincter incompetence in patients with symptomatic gastroesophageal reflux. Mechanoreceptors of the proximal stomach: Role in triggering transient lower esophageal sphincter relaxation. Reappraisal of the flap valve mechanism in the gastroesophageal junction: A study of a new valvuloplasty procedure in cadavers. Intraganglionic laminar endings are mechano-transduction sites of vagal tension receptors in the guinea pig stomach. Esophagogastric junction opening during relaxation distinguishes non-hernia reflux patients, hernia patients and normal subjects. Identification and mechanism of delayed esophageal acid clearance in subjects with hiatus hernia. Assessment of neural inhibition of the lower esophageal sphincter in cats with esophagitis. The effect of hiatal hernia on gastroesophageal reflux disease and influence on proximal and distal esophageal reflux. Hiatus hernia and intrathoracic migration of the esophagogastric junction in gastroesophageal reflux disease. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distension in reflux patients with hiatal hernia. Esophageal shortening induced by short-term intraluminal acid perfusion: A cause for hiatus hernia Unbuffered highly acidic gastric juice exists at the gastroesophageal junction after a meal. Severe reflux disease is associated with an enlarged unbuffered proximal gastric acid pocket. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease.
Older adult patients should not ideally be treated medically and be operated on early for the following reasons: (1) malignancy is more likely blood pressure 800 adalat 20 mg order fast delivery, (2) atrophy of the greater omentum makes spontaneous sealing less likely, (3) such patients often withstand sepsis and organ dysfunction poorly, and (4) early surgery leads to a better outcome in this subgroup. The controversies in the operative management have revolved around the need for a definitive ulcer operation after closure of the perforation (and which definitive operation to perform) and, more recently, the choice between laparoscopic and open repair. Simple closure of a perforated duodenal or a juxtapyloric ulcer with the use of an omental patch is widely practiced. Relapse of ulcer disease with modern medical Angiographic Therapy Angiographic embolization of bleeding arteries is a nonoperative alternative to surgery in patients with bleeding peptic ulcer. In a nonrandomized comparison to surgery, angiographic embolization carried a similar rate of recurrent bleeding (29% vs. Laparoscopic repair was quicker to perform and led to less postoperative pain, a lower analgesic requirement, and a shorter hospitalization time. Boey and associates171 identified preoperative shock, major medical illnesses, and perforation longer than 12 hours as important risk factors. Definitive ulcer surgery (vagotomy and gastrectomy) also led to a higher mortality rates; deaths occurred in older patients who had concomitant ulcer complications. Laparoscopic view of a perforated duodenal ulcer (arrow) with fibrinous exudate on the adjacent peritoneum. There is evidence that Hp eradication reduces relapse of ulceration after patch repair. The optimal treatment of an angular notch ulcer along the lesser curvature of the stomach should entail an antrectomy followed by a Billroth type I gastroduodenostomy. Simple closure should be considered in prepyloric ulcers, especially when they are small. The role of a vagotomy or indeed gastric resection in these prepyloric perforated ulcers is unclear. The arguments for primary resection also include the possibility that the ulcer is malignant. Its clinical manifestations-nausea and postprandial vomiting, abdominal fullness, pain, and early satiety-are discussed in Chapters 15 and 49, as is the diagnostic approach to patients presenting with possible gastric outlet obstruction. Gastric outlet obstruction should alert clinicians to possible malignancy (see Chapter 54). The loss of fluid, hydrogen ions, and chloride ions in the vomitus leads to hypochloremic, hypokalemic metabolic alkalosis. The patient should be volume resuscitated with normal saline followed by potassium replacement once urine output is adequate. A high-volume, nonbile-stained aspirate can help distinguish gastric outlet obstruction from a high small bowel obstruction. Improvement is especially noticeable in patients with active ulceration and edema. Surgery is thus deferred until after an adequate trial of conservative management. Furthermore, many authorities argue for initial endoscopic dilation before surgery. A lowcompliance through-the-scope balloon is then passed over the guidewire, and dilation can be seen through the endoscope. The use of a balloon is preferred because its inflation produces a uniform radial force, which has a theoretical advantage over the longitudinal shearing force associated with the use of conventional dilators. The targeted diameter is unclear; many authorities recommend dilation to 15 mm, which is often associated with relief of symptoms. B, A waist, representing the stricture (arrow), was observed and was nearly abolished on balloon inflation (C). In a small series of Hp-infected patients, balloon dilation followed by Hp eradication led to sustained symptom relief. They include truncal vagotomy with either a drainage procedure (gastrojejunostomy or pyloroplasty) or an antrectomy. Surgical management principles for gastric outlet obstruction were established in an era when (1) this peptic complication was common, (2) recurrence was likely without definitive surgical therapy, (3) potent antisecretory therapy and endoscopic dilation techniques were not available, and (4) parenteral nutrition options were limited. Therefore, an immediate decision regarding the need for surgery is generally not necessary for a patient who presents with gastric outlet obstruction. The problem can be managed with medical and endoscopic means in approximately 70% of cases, and only 30% eventually require 1 of the previously mentioned operations to bypass the gastric outlet obstruction. The approach to treatment of actively bleeding stress ulcers is similar to that of bleeding peptic ulcers, already discussed. However, the risk of recurrent bleeding is high, and bleeding carries a high mortality rate due to multi-organ failure. Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding. High incidence of mortality and recurrent bleeding in patients with Helicobacter pylori-negative idiopathic bleeding ulcers. Helicobacter pylori "test-and-treat" strategy for management of dyspepsia: A comprehensive review. Gastrointestinal safety of cyclooxygenase-2 inhibitors: A Cochrane collaboration systematic review. Combination of a cyclo-oxygenase-2 inhibitor and a proton pump inhibitor for prevention of recurrent ulcer bleeding in patients at very high risk: A double-blind randomized trial. Cardiovascular risk and inhibition of cyclooxygenase: A systematic review of the observational studies of selective and nonselective inhibitors of cyclooxygenase 2. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Unidentified curved bacilli in the stomachs of patients with gastritis and peptic ulcer. Causes underlying the birth-cohort phenomenon of peptic ulcer: Analysis of mortality data 1911-2000, England and Wales.