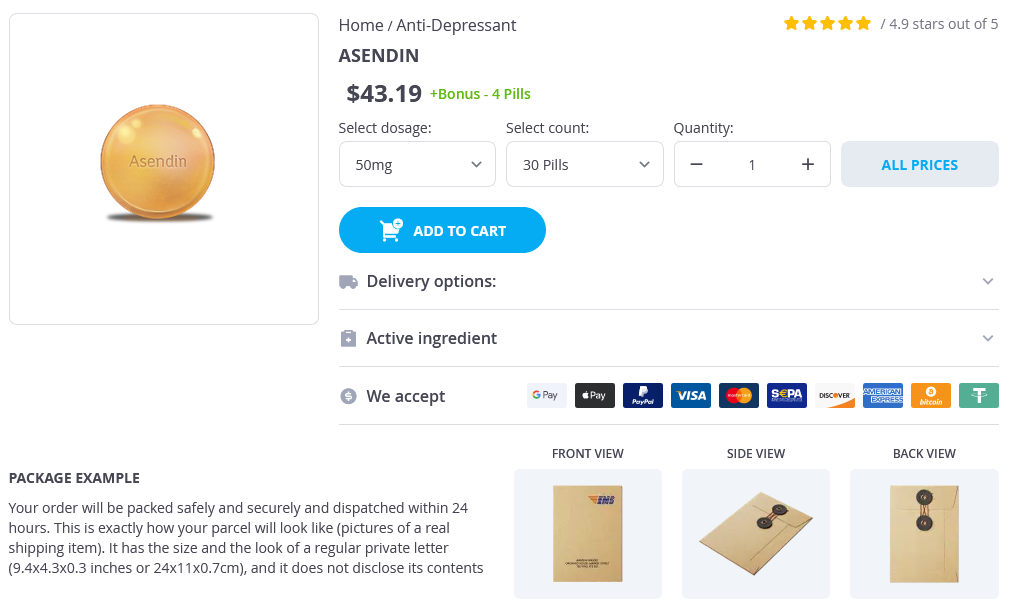
Asendin Dosage and Price
Asendin 50mg
- 30 pills - $47.99
- 60 pills - $84.99
- 90 pills - $118.69
- 120 pills - $154.65
- 180 pills - $223.19
- 360 pills - $434.99
Diagnosis of ventilator-associated pneumonia by bacteriologic analysis of bronchoscopic and nonbronchoscopic "blind" bronchoalveolar lavage fluid anxiety meaning purchase discount asendin line. The value of pretest probability and modified clinical pulmonary infection score to diagnose ventilator-associated pneumonia. Diagnosing pneumonia during mechanical ventilation: the clinical pulmonary infection score revisited. Impact of inappropriate antibiotic therapy on mortality in patients with ventilatorassociated pneumonia and blood stream infection: a metaanalysis. Impact of invasive and noninvasive quantitative culture sampling on outcome of ventilator-associated pneumonia: a pilot study. Impact of quantitative invasive diagnostic techniques in the management and outcome of mechanically ventilated patients with suspected pneumonia. Invasive and noninvasive strategies for management of suspected ventilatorassociated pneumonia. Quantitative versus qualitative cultures of respiratory secretions for clinical outcomes in patients with ventilator-associated pneumonia. Pathogens in the lower respiratory tract of intensive care unit patients: impact of duration of hospital care and mechanical ventilation. Significance of the isolation of Candida species from respiratory samples in critically ill, non-neutropenic patients. The significance of distal bronchial samples with commensals in ventilator-associated pneumonia: colonizer or pathogen Both early-onset and late-onset ventilator-associated pneumonia are caused mainly by potentially multiresistant bacteria. The impact of antimicrobial-resistant, health care-associated infections on mortality in the United States. Antimicrobialresistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the Centers for Disease Control and Prevention, 2009-2010. Acinetobacter baumannii ventilator-associated pneumonia: epidemiological and clinical findings. The effect of late-onset ventilator-associated pneumonia in determining patient mortality. Methicillinresistant Staphylococcus aureus prolongs intensive care unit stay in ventilator-associated pneumonia, despite initially appropriate antibiotic therapy. Respiratory viruses in bronchoalveolar lavage: a hospital-based cohort study in adults. Disruption of services in an internal medicine unit due to a nosocomial influenza outbreak. Reduction of fluoroquinolone use is associated with a decrease in methicillin-resistant Staphylococcus aureus and fluoroquinolone-resistant Pseudomonas aeruginosa isolation rates: a 10 year study. Variations in etiology of ventilator-associated pneumonia across four treatment sites: implications for antimicrobial prescribing practices. Incidence and susceptibility of pathogenic bacteria vary between intensive care units within a single hospital: implications for empiric antibiotic strategies. Previous endotracheal aspirate allows guiding the initial treatment of ventilator-associated pneumonia. The role of anaerobes in patients with ventilator-associated pneumonia and aspiration pneumonia: a prospective study. Linezolid limits burden of methicillin-resistant Staphylococcus aureus in biofilm of tracheal tubes. Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: a systematic review and meta-analysis. Clinical outbreak of linezolid-resistant Staphylococcus aureus in an intensive care unit. Clinical cure and survival in gram-positive ventilator-associated pneumonia: retrospective analysis of two double-blind studies comparing linezolid with vancomycin. Relationship of vancomycin minimum inhibitory concentration to mortality in patients with methicillin-resistant Staphylococcus aureus hospital-acquired, ventilator-associated, or healthcare-associated pneumonia. Impact of vancomycin exposure on outcomes in patients with methicillin-resistant Staphylococcus aureus bacteremia: support for consensus guidelines suggested targets. Effect of vancomycin plus rifampicin in the treatment of nosocomial methicillinresistant Staphylococcus aureus pneumonia. Pseudomonas aeruginosa bloodstream infection: importance of appropriate initial antimicrobial treatment. Optimal management therapy for Pseudomonas aeruginosa ventilator-associated pneumonia: an observational, multicenter study comparing monotherapy with combination antibiotic therapy. Efficacy and safety evaluation of fixed dose combination of cefepime and amikacin in comparison with cefepime alone in treatment of nosocomial pneumonia patients. Aerosolized antibiotics for ventilator-associated pneumonia: lessons from experimental studies. Inhaled colistin as adjunctive therapy to intravenous colistin for the treatment of microbiologically documented ventilatorassociated pneumonia: a comparative cohort study. Aerosolized plus intravenous colistin versus intravenous colistin alone for the treatment of ventilator-associated pneumonia: a matched case-control study. Randomized controlled trial of nebulized colistimethate sodium as adjunctive therapy of ventilator-associated pneumonia caused by gram-negative bacteria. Nebulized ceftazidime and amikacin in ventilator-associated pneumonia caused by Pseudomonas aeruginosa.
Management of drug and food interactions with azole antifungal agents in transplant recipients depression symptoms without sadness order 50 mg asendin visa. Pharmacokinetics of posaconazole coadministered with antacid in fasting or nonfasting healthy men. Pharmacokinetics, safety, and tolerability of oral posaconazole administered in single and multiple doses in healthy adults. Successful treatment of rhinocerebral mucormycosis by a combination of aggressive surgical debridement and the use of systemic liposomal amphotericin B and local therapy with nebulized amphotericin-a case report. Hyperbaric oxygen therapy for cutaneous/soft-tissue zygomycosis complicating diabetes mellitus. Interferon- gamma and granulocyte-macrophage colonystimulating factor augment the activity of polymorphonuclear leukocytes against medically important zygomycetes. Hyperbaric oxygen as an adjunct in zygomycosis: randomized controlled trial in a murine model. Interferon-gamma and colonystimulating factors as adjuvant therapy for refractory fungal infections in children. Current status of granulocyte (neutrophil) transfusion therapy for infectious diseases. Gastrointestinal basidiobolomycosis in Arizona: clinical and epidemiological characteristics and review of the literature. Basidiobolomycosis: an unusual fungal infection mimicking inflammatory bowel disease. Rhinofacial zygomycosis caused by Conidiobolus coronatus: a case report including in vitro sensitivity to antimycotic agents. Entomophthoramycosis: therapeutic success by using amphotericin B and terbinafine. Sporotrichosis usually begins when the causative agent, Sporothrix schenckii, is inoculated into a site of a minor skin injury and produces an ulcerated, verrucous, or erythematous nodule, sometimes associated with local lymphatic spread. On rare occasions the fungus is inhaled and causes a granulomatous pneumonitis that often cavitates, producing a clinical pattern similar to tuberculosis. Colonies are initially white but gradually become brown to black due to the production of pigmented conidia. In vivo or at 37° C on rich media such as brain-heart infusion, the organism converts to an oval- or cigar-shaped budding yeast. Along with the characteristic morphology of the sporulating mold, identification is based on demonstration of this conversion to a yeast form. Sporotrichosis has been reported from locations around the globe, but most case reports come from the tropical and subtropical regions of the Americas. Cases of animal-to-human transmission involving squirrels, horses, dogs, cats, pigs, mules, insects, and birds have been described. Cutaneous disease arises at sites of minor trauma and inoculation of the fungus into the skin. The initial lesion is most often on a distal extremity, but almost any site may be involved, including such central locations as the nose and the ocular adnexa. The lesions may be smooth or verrucous, and they often ulcerate and develop raised erythematous borders. Secondary lesions do not usually involve a lymph node, although lymphadenopathy may develop. The fixed, or plaque, form of sporotrichosis differs by not demonstrating any tendency to spread locally. Although spontaneous resolution of fixed sporotrichosis has been described,12 the lesions of sporotrichosis usually wax and wane over months to years. The patient will not have systemic symptoms and laboratory examinations will be normal. Cultures of the drainage from skin lesions are occasionally helpful, but culture of biopsy material is preferred and is diagnostic when positive. Microscopic examination will reveal pyogranulomas in the mid and upper dermis, but examination of multiple sections may be required in order to demonstrate the organism. The joint is swollen and painful on motion, an effusion is present, and a sinus tract may develop. Systemic symptoms are minimal and, other than elevation of the erythrocyte sedimentation rate, laboratory examinations are unrevealing. Tenosynovitis associated with carpal tunnel syndrome or nerve entrapment has been reported. Failure to consider the diagnosis has resulted in an average 25-month delay before diagnosis. Differential considerations include pigmented villonodular synovitis, tuberculosis, gout, osteoarthritis, and rheumatoid arthritis. Approximately one third of the patients are alcoholic; one third have another concomitant medical illness such as pulmonary tuberculosis, diabetes mellitus, sarcoidosis, and steroid use; and one third are apparently normal. Patients are occasionally asymptomatic but will usually have a productive cough, low-grade fever, or weight loss. Other than elevation of the erythrocyte sedimentation rate, laboratory abnormalities are minimal. The chest radiograph reveals unilateral or bilateral cavitary lesions, usually with an associated parenchymal infiltrate. Gram stain or cytologic examination of sputum or bronchial washings will sometimes reveal elongated budding yeast,21 and sputum culture will usually yield the organism. With some patients, however, repeated cultures and long-term follow-up are necessary in order to make the diagnosis. A single case of spontaneous resolution of noncavitary infection has been reported.
Factors and outcomes associated with the decision to treat primary pulmonary coccidioidomycosis anxiety herbal remedies purchase asendin amex. Survival improvement in coccidioidal meningitis by high-dose intrathecal amphotericin B. Correlation between antifungal susceptibilities of Coccidioides immitis in vitro and antifungal treatment with caspofungin in a mouse model. Use of the echinocandins (caspofungin) in the treatment of disseminated coccidioidomycosis in a renal transplant recipient. Evaluation of nikkomycins X and Z in murine models of coccidioidomycosis, histoplasmosis, and blastomycosis. Cutaneous Antifungal Agents: Selected Compounds in Clinical Practice and Development. Modeling nikkomycin Z dosing and pharmacology in murine pulmonary coccidioidomycosis preparatory to phase 2 clinical trials. Immunity to coccidioidomycosis induced in mice by purified spherule, arthrospore, and mycelial vaccines. Influence of vaccination on respiratory coccidioidal disease in cynomolgus monkeys. Immunogenic properties of nondisrupted and disrupted spherules of Coccidioides immitis in mice. Immunization of mice to Coccidioides immitis: dose, regimen and spherulation stage of killed spherule vaccines. Enhancement of immune responses in mice by a booster injection of Coccidioides spherules. Resistance of vaccinated mice to typical and atypical strains of Coccidioides immitis. Immunologic responsiveness and safety associated with the Coccidioides immitis spherule vaccine in volunteers of white, black and Filipino ancestry. Valley Fever Vaccine Study Group: evaluation of the protective efficacy of the killed Coccidioides immitis spherule vaccine in humans. Chapter 267 Coccidioidomycosis(CoccidioidesSpecies) 2985 268 Definition Dermatophytosis (Ringworm) and Other Superficial Mycoses Roderick J. The superficial fungal infections include some of the most common infectious conditions, such as ringworm, tinea corporis, and pityriasis versicolor, as well as rare disorders such as tinea nigra. Their prevalence varies in different parts of the world, but in many tropical countries they are the most common causes of skin disease. Dermatophyte infections and other superficial mycoses are described in this chapter. The dermatophytes are molds that can invade the stratum corneum of the skin or other keratinized tissues derived from epidermis, such as hair and nails. They may cause infections (dermatophytoses) at most skin sites, although the feet, groin, scalp, and nails are most commonly affected. Trichophyton schoenleinii, the cause of the scalp infection favus, was isolated from a patient and the culture shown to reproduce the typical lesions after inoculation onto human skin as early as 1841. Dermatophyte infections had been described many years before this, although the identity of the cause had not been recognized. The ancient Greek physicians knew about ringworm, and there are descriptions of the manifestations of dermatophytosis in more unlikely sources, such as the records of the early Dutch explorers of the 16th century who reported a strange disease of the skin, subsequently known as tinea imbricata, caused by Trichophyton concentricum, in the islanders of the western Pacific. These keratinophilic organisms probably arose as saprophytic soil fungi, and some dermatophytes, which have been isolated only from soil, have not been shown to cause disease in either animals or humans. Most of the 39 dermatophyte species, however, are parasitic and can cause disease in either humans or animals, often being adapted to a single or narrow range of host species. The dermatophytes are referred to as zoophilic, anthropophilic, or geophilic, depending on whether their primary source is an animal, human, or soil, respectively. The taxonomy of these fungi is complicated by the fact that most clinical isolates are imperfect fungi (organisms that do not produce sexual structures in culture). However, sexual forms of many of these species are known and have been assigned to one genus, Arthroderma, which corresponds to the imperfect genera Trichophyton and Microsporum. The exact taxonomic status of dermatophytes remains a subject of debate, although the wider use of molecular tools to determine species has enabled a scientifically based classification to evolve. The relationships among different dermatophytes are not simply a subject for intellectual dispute. To understand the spread of infections, for instance, it is important to attempt to differentiate strains of the same species. Significant advances have been made both in the molecular taxonomy of these organisms and in the development of schemes for strain differentiation through the use of molecular tools. Attempts have also been made to classify the dermatophytes according to their protein composition4 and production of antibiotics or enzymes such as urease. Proteinases produced by dermatophytes are inducible by, for instance, amino acids. Zoophilic Dermatophyte Infections the main zoophilic dermatophyte fungi are listed in Table 268-1. Each organism is primarily an animal pathogen that sometimes causes human infection. In each case there is usually a range of host specificities, from organisms such as Microsporum nanum, whose natural host is the pig and which does not infect other animals, to Trichophyton mentagrophytes, which affects a range of different rodent species or, rarely, cats, dogs, and horses.