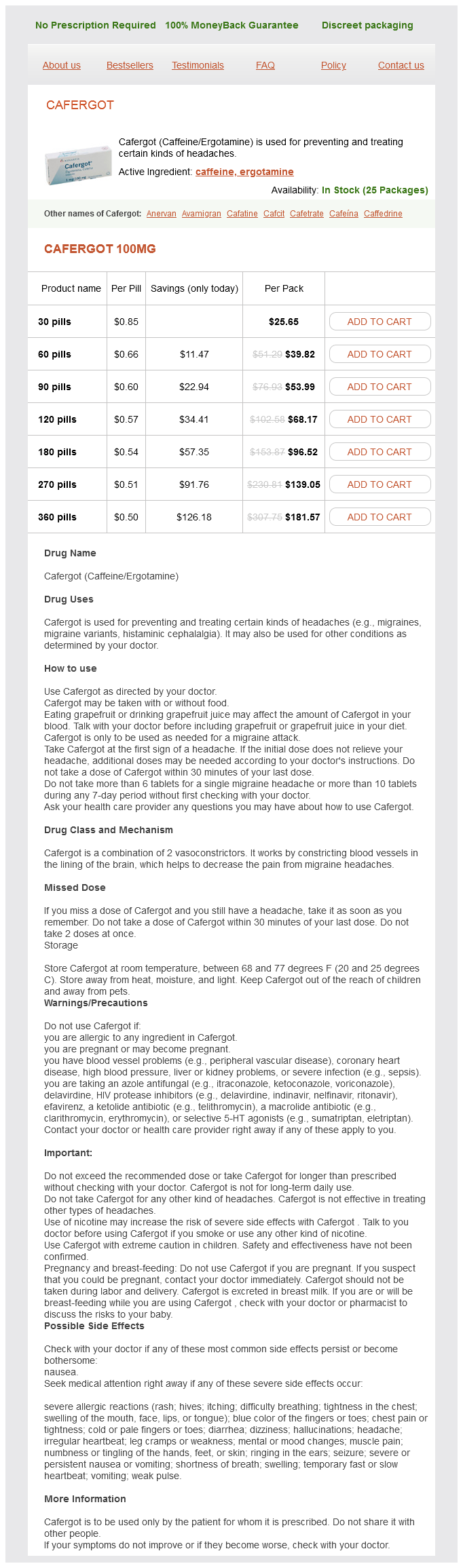
Cafergot Dosage and Price
Cafergot 100mg
- 30 pills - $25.65
- 60 pills - $39.82
- 90 pills - $53.99
- 120 pills - $68.17
- 180 pills - $96.52
- 270 pills - $139.05
- 360 pills - $181.57
In some cases wnc pain treatment center arden nc order cafergot with visa, the lesion is extensive, which makes it difficult to obtain negative margins of excision. Adenosis And sclerosing lesions - 219 TuBulAr AdenoSiS Tubular adenosis is an unusual benign lesion, which may be misinterpreted as carcinoma, particularly tubular carcinoma. Tubular adenosis is composed of a haphazard proliferation of elongated and branching tubules, which have both epithelial and myoepithelial layers. In such cases, the haphazard arrangement of the glands combined with the atypical cytologic features raises particular concern for invasive carcinoma. A: low-power view showing the haphazard proliferation of elongated, branching tubules. A: low-power view illustrating a haphazard, nonlobulocentric proliferation of small glands. B: High-power view demonstrating round to ovoid glands, with intraluminal eosinophilic secretion seen in one of the glands similar to that seen in microglandular adenosis. Some authors have described and illustrated as "blunt duct adenosis" a lesion that appears to represent usual ductal hyperplasia involving lobular acini and terminal ductules. The terms radial scar, radial sclerosing lesion, sclerosing papillary proliferation, and complex sclerosing lesion, among others, have been used for this histologically complex picture. We reserve the term radial scar for those sclerosing lesions characterized by a central, sclerotic nidus from which ducts and lobules radiate circumferentially. Sclerosing lesions with a less organized appearance are categorized as complex sclerosing lesions. Radial scars may be identified as an incidental finding in breast tissue removed for another abnormality or may be large enough to be detected by mammography. The mammographic appearance is typically that of a spiculated mass and can mimic carcinoma. When large enough to be apparent upon gross examination, they appear as firm, chalky white lesions with an irregular stellate outline that may be difficult to distinguish from carcinoma. Microscopically, radial scars show a central area of stromal sclerosis and elastosis containing entrapped and variably distorted glands and epithelial cell nests, an appearance that may simulate invasive carcinoma. However, in our experience, even with immunostains, myoepithelial cells are frequently identifiable only around some of the glands or may show a reduction or even absence of staining for some myoepithelial cell markers. A: low-power view demonstrates a central area of fibroelastotic stroma containing entrapped glands and surrounded by radiating ducts with usual ductal hyperplasia and cystic changes. An outer myoepithelial layer is evident around some of the glands, but this is easier to appreciate on a smooth muscle myosin heavy chain immunostain (c). However, the lesions are often larger and do not have the well-defined radial configuration of radial scars. The histologic features of complex sclerosing lesions show considerable overlap with those of sclerosing papillomas (see Chapter 8); in fact, many such lesions likely represent a late stage of sclerosing papilloma in which the distortion of the underlying papillary structure precludes its recognition. As for sclerosing adenosis, involvement of radial scars and complex sclerosing lesions by in situ carcinoma results in the appearance of neoplastic epithelial cells within a fibrotic stroma. B: High-power view of glands from the sclerotic area shows that they are surrounded by a myoepithelial cell layer. However, as for radial scars, the myoepithelial cells surrounding the glands within complex sclerosing lesions may show a reduction or absence of expression of one or more myoepithelial cell markers. Studies that have assessed the frequency with which a worse lesion is found on excision following a core-needle biopsy diagnosis of radial scar have been limited by small patient numbers and possible selection bias. Most authorities agree, however, that the finding of radial scar on a core-needle biopsy is an indication for excision. Atypical apocrine adenosis of the breast: a clinicopathologic study of 37 patients with 8. Carcinoma arising in microglandular adenosis: an immunohistochemical analysis of 20 intraepithelial and invasive neoplasms. Microglandular adenosis with transition to breast carcinoma: a series of three cases. Microglandular adenosis with transition in to adenoid cystic carcinoma of the breast. Mammographic lesions suggestive of radial scars: microscopic findings in 40 cases. Carcinoma and atypical hyperplasia in radial scars and complex sclerosing lesions: importance of lesion size and patient age. Interdependence of radial scar and proliferative disease with respect to invasive breast cancer risk in benign breast biopsies. Percutaneous core needle biopsy of radial scars of the breast: when is excision necessary Radial scar lesions of the breast diagnosed by needle core biopsy: analysis of cases containing occult malignancy. Stereotactic, automated, large-core needle biopsy of nonpalpable breast lesions: falsenegative and histologic underestimation rates after long-term follow-up. Follow-up of breast lesions diagnosed as benign with stereotactic core-needle biopsy: frequency of mammographic change and false-negative rate. A review of needle core biopsy diagnosed radial scars in the Welsh Breast Screening Programme. Radial scars without atypia diagnosed at imagingguided needle biopsy: how often is associated malignancy found at subsequent surgical excision, and do mammography and sonography predict which lesions are malignant These lesions have in common a growth pattern characterized by the presence of finger-like projections or fronds of variable length and thickness that are composed of central fibrovascular cores covered by epithelium. First, as will be discussed in more detail, assessment of the presence and distribution of myoepithelial cells in the lesion is one of the most helpful features in arriving at the correct diagnosis (Table 8. In some cases, this may require the use of immunostains to myoepithelial cell proteins. Second, the ideal method to examine an excisional biopsy specimen containing a suspected intraductal papillary lesion involves carefully opening the involved duct longitudinally using a pair of fine scissors until the tumor is exposed. Identification of the lesion may be facilitated by the surgeon placing a suture at the end of the involved duct nearest the nipple.
Obstructing malignant tumor of trachea pain treatment center winnipeg purchase cafergot online pills, bronchus and esophagus Vascular lesions: Hereditary hemorrhagic telangiectasia of nose Lymphatic disorders: Lymphangioma. The utmost caution is required to prevent accidents, which can injure not only patient but also health care personnel present in operation room. Nursing and operation theater personnel should be conversant with safety measures while operating laser. Protection of skin: All exposed parts of the patient not in surgical field, which include skin, mucous membranes and teeth, are protected by saline soaked towels, pads or sponges that are moistened periodically. Evacuation of smoke: Two separate suctions, one for the blood and mucous and the other for smoke and steam (produced by laser vaporization of tissues) are used. Anesthetic gases and equipment: the endotracheal tube fire is the dreaded complication. It can be used in the following disorders: related disciplines Nasal obstruction: Reduction of hypertrophied inferior turbinates. Lingual thyroid Tonsillotomy Microlaryngeal surgery to remove granuloma, papilloma and cyst Myringotomy Rhinophyma Cosmetic: Removal of skin lesions. The parameters, which can be controlled by the device, include: Power in watts Temperature in degrees of celsius Resistance in ohms Treatment time in seconds Energy in joules (watts × seconds). The probes are available in different sizes and designs and produce a tip temperature of 70°C. The thermocouples of probes can be inserted in to the tissue to monitor the temperature. Urea and dissolved gases increase to reach toxic concentrations, which cause cell death. Cryosurgery is useful in the treatment of vascular lesions (hemangioma, angiofibroma and glomus tumors) because thrombosis of capillaries results in less bleeding. Autoantibodies specific to the frozen tumor tissues may provide tissue specific immunity to subsequent recurrence. Thermocouple: If available, a thermocouple will ensure freezing at an adequate depth. Cryotherapy does not cause indications Hyperbaric oxygen has been used with success in following disorders: 1. Sudden idiopathic sensorineural hearing loss and tinnitus: the results are better if therapy is started earlier. The cryoprobe is kept for 38 minutes so that area is frozen rapidly reaching a temperature of about 70°C. Section 9 w related disciplines Appendix Today the human body is, tomorrow it is not; even the shortest span of life is beset with pain and misery. They are responsible for generating the cochlear microphonic and otoacoustic emissions. Subjective tinnitus: It is most common type of tinnitus and is heard only by the patient. Conductive hearing loss: the most common causes are ear wax, otitis media, otomycosis, and otosclerosis. Patient has conductive hearing loss with normal tympanic membrane and impaired acoustic reflexes. Reversible causes of sensorineural hearing loss: They must be ruled out even in patients with the most common causes of hearing loss. Mild hearing loss in children: Address even mild hearing loss early to prevent speech delay in children. Otoscopy may show a "trail sign" of debris along the posterosuperior canal wall to the marginal perforation. Dix-Hallpike examination: It is the most important clinical test for dizzy patients because 25% of all dizzy patients have benign paroxysmal positioning vertigo. Downbeating nystagmus: A pure downbeating nystagmus during Dix-Hallpike testing suggests Chiari malformation or other posterior fossa lesions. Peripheral and central vertigo: Patients with central dizziness complain few symptoms but have many findings (sensory/motor deficits). Patients with peripheral vertigo have many symptoms (severe whirling vertigo with or without otological symptoms) but few findings. Facial nerve: the regeneration and degree of return to normal is dependent on the degree of initial injury (neuropraxia vs. The most important factor in history is whether the palsy develops slowly over days or immediately at the time of the injury. Indications for surgical exploration of the facial nerve in temporal bone fracture: They include: a. Anosmia: the three most common causes are sinonasal disease, post-upper respiratory tract infection and trauma (injury to olfactory nerves at cribriform plate or brain injury). Antibiotic resistance patterns in acute bacterial rhinosinusitis: Penicillin resistant Streptococcus pneumoniae (2540%), beta lactamase producing Haemophilus influenzae (3040%) and beta lactamase producing Moraxella catarrhalis (92%). Chronic hyperplastic rhinosinusitis: Eosinophilic infiltration is the hallmark in most of the patients and about 50% of patients have asthma. Polychondritis: Seventy to eighty percent patients have involvement of the nasal septum. Blood loss: Young healthy patients can lose up to 30% of blood volume with minimal symptoms. Intubation: It is required if the patient has Glasgow Coma Scale score of 8 or less. Other options include healing by secondary intention, local flaps, skin grafts and regional or free flaps.
The first steps can be catalyzed by glutathione transferase treatment for residual shingles pain cafergot 100 mg buy with mastercard, or they can occur nonenzymatically. Recycling through these counteracting enzyme systems, a process known as retro-reduction or futile cycling (Hinrichs et al. Sulfoxide reduction may also occur nonenzymatically at an appreciable rate, as in the case of the proton pump inhibitor rabeprazole (Miura et al. Bioreductive alkylating agents, which include such drugs as mitomycins, anthracyclins, and aziridinylbenzoquinones, represent another class of anticancer agents that require activation by reduction. Biotransformation of disulfiram by disulfide reduction (A) and the general mechanism of glutathione-dependent disulfide reduction of xenobiotics (B). In the latter reaction, two molecules of gluathione are oxidized with reduction of the sulfine oxygen to water (Madan et al. The two-electron reduction of quinones is a nontoxic reaction-one that is not associated with semiquinone formation and oxidative stress-provided the resultant hydroquinone is sufficiently stable to undergo glucuronidation or sulfonation. Note that tirapazamine (3-amino-1,2,4-benzotriazine-1,4-dioxide) is a representative of a class of agents that are activated by reduction, which may be clinically useful in the treatment of certain tumors. Two-electron reduction of menadione to a hydroquinone, and production of reactive oxygen species during its 1-electron reduction to a semiquinone radical. Oxidative stress is an important component to the mechanism of toxicity of several xenobiotics that either contain a quinone or can be biotransformed to a quinone (Anders, 1985). The production of superoxide anion radicals and oxidative stress are responsible, at least in part, for the cardiotoxic effects of doxorubicin (adriamycin) and daunorubicin (daunomycin), the pulmonary toxicity of paraquat and nitrofurantoin, and the neurotoxic effects of 6-hydroxydopamine. Oxidative stress also plays an important role in the destruction of pancreatic cells by alloxan and dialuric acid. Tissues, low in superoxide dismutase activity, such as the heart, are especially susceptible to the oxidative stress associated with the redox cycling of quinones. This accounts, at least in part, for the cardiotoxic effects of adriamycin and related anticancer agents, although other susceptibility factors have been proposed (Mordente et al. Hydroquinones formed by two-electron reduction of unsubstituted or methyl-substituted 1,4-naphthoquinones (such as menadione) or the corresponding quinone epoxides are relatively stable to autoxidation, whereas the methoxyl, glutathionyl, and hydroxyl derivatives of these compounds undergo autoxidation with production of semiquinones and reactive oxygen species. The glutathione conjugates of quinones can also be reduced to hydroquinones by carbonyl reductases, which actually have a binding site for glutathione. In human carbonyl reductase, this binding site is Cys227, which is involved in binding both substrate and glutathione (Tinguely and Wermuth, 1999). These electrophilic and redox active metabolites activate Nrf2 and induce various enzymes that protect against oxidative stress. One isothiocyanate in particular, phenethyl isothiocyanate, has been found to activate Nrf2 and activate numerous genes in addition to those encoding xenobiotic-biotransforming enzymes and oxidant defense systems. As with other xenosensors, activation of Nrf2 results in a pleiotypic response in which a large number of genes are activated (or repressed). The hematotoxicity of benzene is thought to involve its conversion to hydroquinone in the liver and its subsequent oxidation to benzoquinone by myeloperoxidase in the bone marrow (discussed later in the section "PeroxidaseDependent Cooxidation"). Reduction of 5-fluorouracil by dihydropyrimidine dehydrogenase and its inhibition (suicide inactivation) by sorivudine. Note: Inhibition of dihydropyrimidine dehydrogenase is the mechanism of fatal interactions between sorivudine and the 5-fluorouracil prodrug, tegafur. The mechanism of the lethal interaction between sorivudine and tegafur is illustrated in. The enzyme is located mainly in liver cytosol, where it catalyzes the reduction of 5-fluorouracil and related pyrimidines. Reductive dehalogenation of carbon tetrachloride to a trichloromethyl free radical that initiates lipid peroxidation. In the second mechanism, known as oxidative dehalogenation, a halogen and hydrogen on the same carbon atom are replaced with oxygen. These reactions play an important role in the biotransformation and metabolic activation of several halogenated alkanes, as the following examples illustrate. Halothane can also be converted by reductive dehalogenation to a carbon-centered radical, as shown in. Activation of halothane by reductive and oxidative dehalogenation and their role in liver toxicity in rats and humans. Both the oxidative and reductive pathways of halothane metabolism generate reactive intermediates capable of binding to proteins and other cellular macromolecules. The relative importance of these two pathways to halothane-induced hepatotoxicity is species dependent. In contrast to the situation in rats, halothane-induced hepatotoxicity in guinea pigs is largely the result of oxidative dehalogenation of halothane (Lunam et al. Halothane hepatitis in humans is a rare but severe form of liver necrosis associated with repeated exposure to this volatile anesthetic. In humans, as in guinea pigs, halothane hepatotoxicity results from the oxidative dehalogenation of halothane, as shown in. Serum samples from patients suffering from halothane hepatitis contain antibodies directed against neoantigens formed by the trifluoroacetylation of proteins. These antibodies have been used to identify which specific proteins in the endoplasmic reticulum are targets for trifluoroacetylation during the oxidative dehalogenation of halothane (Pohl et al. In other words, these halogenated aliphatic hydrocarbons, like halothane, may be converted to acylhalides that form immunogens by binding covalently to proteins. In addition to accounting for rare instances of enflurane hepatitis, this mechanism of hepatotoxicity can also account for reports of a cross-sensitization between enflurane and halothane, in which enflurane causes liver damage in patients previously exposed to halothane. One of the metabolites generated from the reductive dehalogenation of halothane is 2-chloro-1,1-difluoroethylene. The formation of this metabolite involves the loss of two halogens from adjacent carbon atoms with formation of a carboncarbon double bond.