Cardizem Dosage and Price
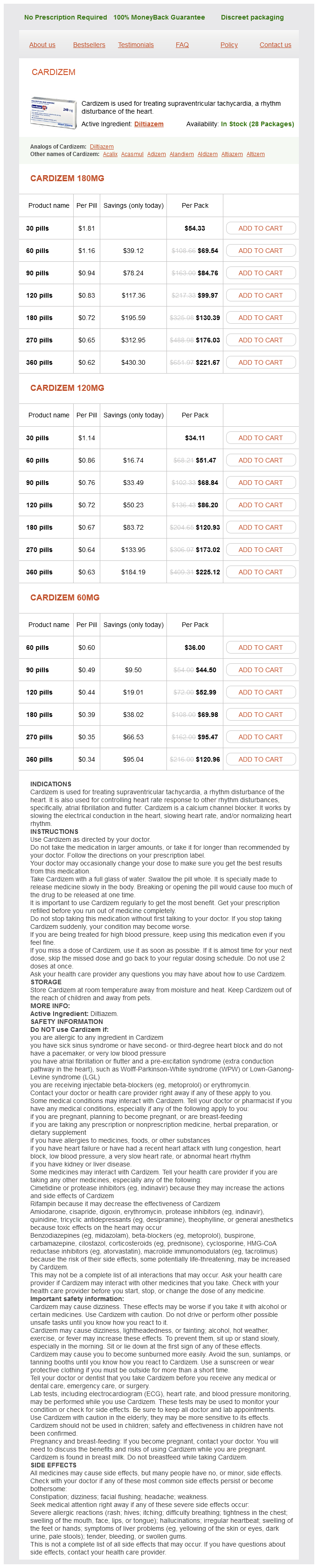
Cardizem 180mg
- 30 pills - $54.33
- 60 pills - $69.54
- 90 pills - $84.76
- 120 pills - $99.97
- 180 pills - $130.39
- 270 pills - $176.03
- 360 pills - $221.67
Cardizem 120mg
- 30 pills - $34.11
- 60 pills - $51.47
- 90 pills - $68.84
- 120 pills - $86.20
- 180 pills - $120.93
- 270 pills - $173.02
- 360 pills - $225.12
Cardizem 60mg
- 60 pills - $36.00
- 90 pills - $44.50
- 120 pills - $52.99
- 180 pills - $69.98
- 270 pills - $95.47
- 360 pills - $120.96
The anal canal arrhythmia heart order 120 mg cardizem free shipping, surrounded by internal and external anal sphincters, descends postero-inferiorly between the anococcygeal ligament and the perineal body. Its contraction (tonus) is stimulated and maintained by sympathetic fibers from the superior rectal (peri-arterial) and hypogastric plexuses. Its contraction is inhibited by parasympathetic fiber stimulation, both intrinsically in relation to peristalsis and extrinsically by fibers conveyed by the pelvic splanchnic nerves. This sphincter is tonically contracted most of the time to prevent leakage of fluid or flatus; however, it relaxes (is inhibited) temporarily in response to distension of the rectal ampulla by feces or gas, requiring voluntary contraction of the puborectalis muscle and external anal sphincter if defecation or flatulence is to be prevented. The ampulla relaxes after initial distension (when peristalsis subsides) and tonus returns until the next peristalsis, or until a threshold level of distension occurs, at which point inhibition of the sphincter is continuous until distension is relieved. The external anal sphincter is a large voluntary sphincter that forms a broad band on each side of the inferior two thirds of the anal canal. The external anal sphincter is described as having subcutaneous, superficial, and deep parts; these are zones rather than muscle bellies and are often indistinct. The external anal sphincter is supplied mainly by S4 through the inferior rectal nerve. Internally, the superior half of the mucous membrane of the anal canal is characterized by a series of longitudinal ridges called anal columns. These columns contain the terminal branches of the superior rectal artery and vein. The anorectal junction, indicated by the superior ends of the anal columns, is where the rectum joins the anal canal. At this point, the wide rectal ampulla abruptly narrows as it traverses the pelvic diaphragm. When compressed by feces, the anal sinuses exude mucus, which aids in evacuation of feces from the anal canal. The inferior comb-shaped limit of the anal valves forms an irregular line, the pectinate line (dentate line). The anal canal superior to the pectinate line differs from the part inferior to the pectinate line in its histology, arterial supply, innervation, and venous and lymphatic drainage. These differences result from the different embryological origins of the superior and inferior parts of the anal canal (Moore et al. The superior rectal artery supplies the anal canal superior to the pectinate line. The two inferior rectal arteries supply the anal canal inferior to the pectinate line as well as the surrounding muscles and peri-anal skin. The middle rectal arteries assist with the blood supply to the anal canal by forming anastomoses with the superior and inferior rectal arteries. The internal rectal venous plexus drains in both directions from the level of the pectinate line. Superior to the pectinate line, the internal rectal plexus drains chiefly into the superior rectal vein (a tributary of the inferior mesenteric vein) and the portal system. Inferior to the pectinate line, the internal rectal plexus drains into the inferior rectal veins (tributaries of the caval venous system) around the margin of the external anal sphincter. The middle rectal veins (tributaries of the internal iliac veins) mainly drain the muscularis externa of the ampulla and form anastomoses with the superior and inferior rectal veins. The normal submucosa of the anorectal junction is markedly thickened and in section has the appearance of a cavernous (erectile) tissue, owing to the presence of the sacculated veins of the internal rectal venous plexus. The vascular submucosa is especially thickened in the left lateral, right anterolateral, and right posterolateral positions, forming anal cushions, or threshold pads, at the point of closure of the anal canal. Inferior to the pectinate line, the lymphatic vessels drain superficially into the superficial inguinal lymph nodes, as does most of the perineum. The nerve supply to the anal canal superior to the pectinate line is visceral innervation from the inferior hypogastric plexus, involving sympathetic, parasympathetic, and visceral afferent fibers. Parasympathetic fibers inhibit the tonus of the internal sphincter and evoke peristaltic contraction for defecation. The superior part of the anal canal, like the rectum superior to it, is inferior to the pelvic pain line (see Table 6. All visceral afferents travel with the parasympathetic fibers to spinal sensory ganglia S2S4. Superior to the pectinate line, the anal canal is sensitive only to stretching, which evokes sensations at both the conscious and unconscious (reflex) levels. For example, distension of the rectal ampulla inhibits (relaxes) the tonus of the internal sphincter. The nerve supply of the anal canal inferior to the pectinate line is somatic innervation derived from the inferior anal (rectal) nerves, branches of the pudendal nerve. Therefore, this part of the anal canal is sensitive to pain, touch, and temperature. Somatic efferent fibers stimulate contraction of the voluntary external anal sphincter. The perineal body is an important structure, especially in women, because it is the final support of the pelvic viscera, linking muscles that extend across 1477 the pelvic outlet, like crossing beams supporting the overlying pelvic diaphragm. The perineal body can be disrupted by trauma (including an inadequately repaired episiotomy), inflammatory disease, and infection, which may result in the formation of a fistula (abnormal canal) connected to the vestibule of the vagina (see the Clinical Box "Vaginal Fistulae"). Urethrocele: Prolapse of the lower anterior vaginal wall that involves only the urethra. Cystocele: Prolapse of the anterior vaginal wall involving the bladder (see the previous Clinical Box "Cystocele, Urethrocele, and Urinary 1478 Incontinence"). Enterocele: Prolapse of the upper posterior vaginal wall involving the rectovaginal pouch.
The ligaments raise folds of peritoneum (medial umbilical folds) on the deep surface of the anterior abdominal wall (see Chapter 2 prehypertension at 36 weeks pregnant discount cardizem 60 mg with mastercard, Back). Postnatally, the patent parts of the umbilical arteries run antero-inferiorly between the urinary bladder and the lateral wall of the pelvis. The origin of the obturator artery is variable; usually, it arises close to the origin of the umbilical artery, where it is crossed by the ureter. It runs antero-inferiorly on the obturator fascia on the lateral wall of the pelvis and passes between the obturator nerve and vein. Within the pelvis, the obturator artery gives off muscular branches, a nutrient artery to the ilium, and a pubic branch. It ascends on the pelvic surface of the pubis to anastomose with its fellow of the opposite side and the pubic branch of the inferior epigastric artery, a branch of the external iliac artery. In a common variation (20%), an aberrant or accessory obturator artery arises from the inferior epigastric artery and descends into the pelvis along the usual route of the pubic branch. The extrapelvic distribution of the obturator artery is described with the lower limb (Chapter 7). In females, it may occur-with nearly equal frequency-as a separate branch of the internal iliac artery or as a branch of the uterine artery. The uterine artery is an additional branch of the internal iliac artery in females, usually arising separately and directly from the internal iliac artery. It descends on the lateral wall of the pelvis, anterior to the internal iliac artery, 1344 and passes medially to reach the junction of the uterus and vagina, where the cervix (neck) of the uterus protrudes into the superior vagina. The relationship of ureter to artery is often remembered by the phrase "water (urine) passes under the bridge (uterine artery). On reaching the side of the cervix, the uterine artery divides into a smaller descending vaginal branch, which supplies the cervix and vagina, and a larger ascending branch, which runs along the lateral margin of the uterus, supplying it. The ascending branch bifurcates into ovarian and tubal branches, which continue to supply the medial ends of the ovary and uterine tube and anastomose with the ovarian and tubal branches of the ovarian artery. The origin of the arteries from the anterior division of the internal iliac artery and distribution to the uterus and vagina are shown. The anastomoses between the ovarian and tubal branches of the ovarian and uterine arteries and between the vaginal branch of the uterine artery and the vaginal artery provide potential pathways of collateral circulation. These communications occur, and the ascending branch courses, between the layers of the broad ligament. It often arises from the initial part of the uterine artery instead of arising directly from the anterior division. The vaginal artery supplies numerous 1345 branches to the anterior and posterior surfaces of the vagina. The middle rectal artery may arise independently from the internal iliac artery, or it may arise in common with the inferior vesical artery or the internal pudendal artery. The internal pudendal artery, larger in males than in females, passes inferolaterally, anterior to the piriformis muscle and sacral plexus. It leaves the pelvis between the piriformis and coccygeus muscles by passing through the inferior part of the greater sciatic foramen. The internal pudendal artery then passes around the posterior aspect of the ischial spine or the sacrospinous ligament and enters the ischio-anal fossa through the lesser sciatic foramen. The internal pudendal artery, along with the internal pudendal veins and branches of the pudendal nerve, passes through the pudendal canal in the lateral wall of the ischio-anal fossa. As it exits the canal, medial to the ischial tuberosity, the internal pudendal artery divides into its terminal branches, the perineal artery and dorsal arteries of the penis or clitoris. The inferior gluteal artery is the larger terminal branch of the anterior division of the internal iliac artery. It passes posteriorly between the sacral nerves (usually S2 and S3) and leaves the pelvis through the inferior part of the greater sciatic foramen, inferior to the piriformis muscle. It supplies the muscles and skin of the buttocks and the posterior surface of the thigh. When the internal iliac artery divides into anterior and posterior divisions, the posterior division typically gives rise to the following three parietal arteries. Within the fossa, the artery divides into an iliac branch, which supplies the iliacus muscle and ilium, and a lumbar branch, which supplies the psoas major and quadratus lumborum muscles. Lateral sacral arteries: Superior and inferior lateral sacral arteries may arise as independent branches or via a common trunk. The lateral sacral arteries pass medially and descend anterior to the sacral anterior rami, giving off spinal branches, which pass through the anterior sacral foramina and supply 1346 the spinal meninges enclosing the roots of the sacral nerves. Some branches of these arteries pass from the sacral canal through the posterior sacral foramina and supply the erector spinae muscles of the back and the skin overlying the sacrum. Superior gluteal artery: the largest branch of the posterior division, the superior gluteal artery supplies the gluteal muscles in the buttocks. As it passes inferiorly, the ovarian artery adheres to the parietal peritoneum and runs anterior to the ureter on the posterior abdominal wall, usually giving branches to it. As the ovarian artery enters the lesser pelvis, it crosses the origin of the external iliac vessels. It then runs medially, dividing into an ovarian branch and a tubal branch, which supply the ovary and uterine tube, respectively. This vessel descends in or near the midline anterior to the bodies of the last one or two lumbar vertebrae and the sacrum and coccyx. During pelvic laparoscopic procedures, it provides a useful indication of the midline on the posterior wall of the pelvis. Before the median sacral artery enters the lesser pelvis, it sometimes gives rise to a pair of L5 arteries. As it descends over the sacrum, the median sacral artery gives off small parietal (lateral sacral) branches that anastomose with the lateral sacral arteries.
The circumflex fibular artery arises from the origin of the anterior or posterior tibial artery at the knee and passes laterally over the neck of the fibula to the anastomoses around the knee blood pressure cuff purchase generic cardizem. It pierces the tibialis posterior, to which it supplies branches, and enters the nutrient foramen in the proximal third of the posterior surface of the tibia. Surface Anatomy of Leg the tibial tuberosity is an easily palpable elevation on the anterior aspect of the proximal part of the tibia, approximately 5 cm distal to the apex of the patella. This oval elevation indicates the level of the head of the fibula and the bifurcation of the popliteal artery into the anterior and posterior tibial arteries. Extensors and flexors of toes are being contracted simultaneously, demonstrating extensor tendons without elevating toes from ground. The patellar ligament may be felt as it extends from the inferior border of the 1734 apex of the patella. When the knee flexes to a right angle, a depression may be felt on each side of the patellar ligament. The head of the fibula is subcutaneous and may be palpated at the posterolateral aspect of the knee, at the level of the tibial tuberosity. The tendon of the biceps femoris may be traced by palpating its distal attachment to the lateral side of the head of the fibula. This tendon and the head and neck of the fibula guide the examining finger to the common fibular nerve. The nerve is indicated by a line along the biceps femoris tendon, posterior to the head of the fibula, and around the lateral aspect of the fibular neck to its anterior aspect, just distal to the fibular head. The anterior border of the tibia is sharp, subcutaneous, and easily followed distally by palpation from the tibial tuberosity to the medial malleolus. The medial surface of the shaft of the tibia is also subcutaneous, except at its proximal end. Its inferior third is crossed obliquely by the great saphenous vein as it passes proximally to the medial aspect of the knee. The shaft of the fibula is subcutaneous only in its distal part, proximal to the lateral malleolus; this is the common site of fractures. Palpate them, noting that the tip of the lateral malleolus extends farther distally and posteriorly than the medial malleolus. The calcaneal tendon can be easily followed to its attachment to the calcaneal tuberosity, the posterior part of the calcaneus. The ankle joint is fairly superficial in the depression on each side of the calcaneal tendon. The heads of the gastrocnemius are easily recognizable in the superior part of the calf of the leg. The soleus can be palpated deep to and at the sides of the superior part of the calcaneal tendon. The soleus can be distinguished from the gastrocnemius during squatting (flexing the knees while standing on toes) because flexion of the knee to approximately 90° makes the gastrocnemius flaccid; plantarflexion in this position is maintained by the soleus. The deep muscles of the posterior compartment are not easily palpated, but their tendons can be observed just posterior to the medial malleolus, especially when the foot is inverted and the toes are flexed. Popliteal abscesses tend to spread superiorly and inferiorly because of the toughness of the popliteal fascia. Popliteal Pulse 1736 Because the popliteal artery is deep, it may be difficult to feel the popliteal pulse. Palpation of this pulse is commonly performed with the person in the prone position with the knee flexed to relax the popliteal fascia and hamstrings. The pulsations are best felt in the inferior part of the fossa where the popliteal artery is related to the tibia. Weakening or loss of the popliteal pulse is a sign of a femoral artery obstruction. Popliteal Aneurysm and Hemorrhage A popliteal aneurysm (abnormal dilation of all or part of the popliteal artery) usually causes edema and pain in the popliteal fossa. A popliteal aneurysm may be distinguished from other masses by palpable pulsations (thrills) and abnormal arterial sounds (bruits) detectable with a stethoscope. Because the artery lies deep to the tibial nerve, an aneurysm may stretch the nerve or compress its blood supply (vasa vasorum). Pain from such nerve compression is usually referred, in this case to the skin overlying the medial aspect of the calf, ankle, or foot. Because the popliteal artery is closely applied to the popliteal surface of the femur and the joint capsule. Furthermore, because of their proximity and confinement within the popliteal fossa, an injury of the artery and vein may result in an arteriovenous fistula (communication between an artery and a vein). Failure to recognize these occurrences and to act promptly may result in the loss of the leg and foot. If the femoral artery must be ligated, blood can bypass the occlusion through the genicular anastomosis and reach the popliteal artery distal to the ligation. Injury to Tibial Nerve Injury to the tibial nerve is uncommon because of its deep and protected position in the popliteal fossa; however, the nerve may be injured by deep lacerations in the fossa. Severance of the tibial nerve produces paralysis of the flexor muscles in the leg and the intrinsic muscles in the sole of the foot. People with a tibial nerve injury are unable to plantarflex their ankle or flex their toes. Containment and Compartmental Infections in Leg Spread of the fascial compartments of the lower limbs are generally closed spaces, ending proximally and distally at the joints. Because the septa and deep fascia of the leg forming the boundaries of the leg compartments are strong, the increased volume consequent to infection with suppuration (formation of pus) increases intracompartmental pressure.