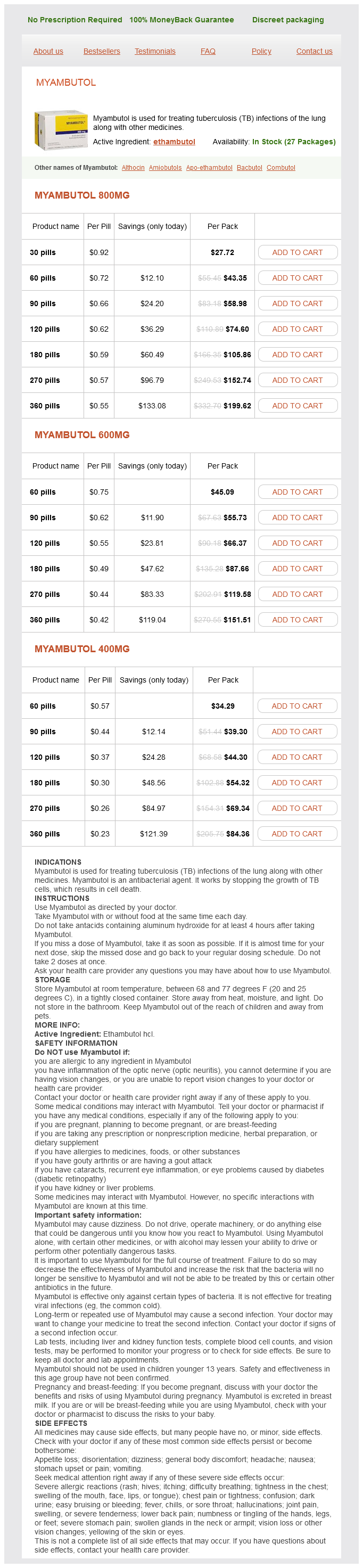
Myambutol Dosage and Price
Myambutol 800mg
- 30 pills - $27.72
- 60 pills - $43.35
- 90 pills - $58.98
- 120 pills - $74.60
- 180 pills - $105.86
- 270 pills - $152.74
- 360 pills - $199.62
Myambutol 600mg
- 60 pills - $45.09
- 90 pills - $55.73
- 120 pills - $66.37
- 180 pills - $87.66
- 270 pills - $119.58
- 360 pills - $151.51
Myambutol 400mg
- 60 pills - $34.29
- 90 pills - $39.30
- 120 pills - $44.30
- 180 pills - $54.32
- 270 pills - $69.34
- 360 pills - $84.36
Curettes the second critical instrument required for the D & C operation is the uterine curette antibiotic resistance microbiome 800 mg myambutol purchase. Several varieties of curettes, including sharp, serrated uterine, and sharp endocervical types, are available. Suction Curettes Suction curettes are manufactured in a variety of sizes, shapes, and curvatures. Dilators the operation of dilatation and curettage (D & C) is one of the most often performed surgical procedures in both obstetrics and gynecology. Baggish Suture Types Sutures are used to close wounds, to secure bleeding vessels, and to seal off visceral structures. A wide variety of suture materials are available, which vary in terms of size, material, content, and consistency. For purposes of explanation, sundry sutures can be divided into absorbable and nonabsorbable. In infected tissues and otherwise dirty areas, absorbable sutures have an advantage in that they provide short-term tensile strength and then disappear. They are less likely to provide a foreign body nidus for continuous inflammation and infection and for subsequent sinus formation. On the other hand, abdominal closure in the face of gross infection is an indication for the use of nonabsorbable suture material, to minimize the risk of dehiscence and/or evisceration. Circle Pop-Off needle and sutures allow the suture to disengage from the needle with a slight tug. A Circle NonPop-Off suture/needle is significantly longer and permits placement of several stitches from the singular length of suture. Most needles used for gynecologic surgery will be 1 2 c (one-half circle) or 5 8 c; the 5 8 c is obviously closer to completing the circle than is the 1 2 c. Suture Selection Suture should be selected on the basis of several parameters: (1) the volume of tissue to be secured, (2) the tensile strength of the tissue to be sutured, and (3) the potential for bacterial contamination. A general guideline that can guide a gynecologic surgeon recommends that the smallest suture that can adequately accomplish the work at hand is the best suture for the job. For example, to select a 0 or 1 suture to secure a small bleeding arteriole deep in the pelvis makes no sense when a 3-0 or 4-0 stitch would suffice. On the other hand, attempting to secure a uterine vessel pedicle or infundibulopelvic ligament pedicle with a 3-0 suture rather than a 0 suture is equally foolhardy. Braided suture has a greater propensity to become contaminated with debris and bacteria within the interstices of the braid compared with monofilament suture. Silk suture is easy to handle and easy to tie down; hence, it forms a secure knot. It should never be used in the urinary bladder and, for that matter, neither should any nonabsorbable suture material. Polyester suture material has all the advantages of silk and better strength and integrity. Polypropylene (Prolene) does not adhere to tissue and is less reactive than nylon. A relatively recent structure concept has been developed by Covidien (New Haven, Conn. At bottom is a reverse cutting needle with the cutting edge positioned on the outer curve of the needle. The V-Loc (polyglyconate) absorbable wound closure suture is barbed to prevent slippage and requires no terminal knot. They end up not uncommonly tying granny knots, which tighten to such an extreme that the tissues strangulate. Regardless of the technique selected, the sine qua non of a good tie-down is a square knot, which does not slip. I prefer these techniques rather than figure-of-8 suturing because the latter, while excellent as a hemostatic stitch, may compromise blood flow, particularly when cinched down tightly. Subcuticular skin closures are commonly used for transverse abdominal incisions and for episiotomy wounds. The two loops are tightened down and do not loosen during the maneuver of completing the second throw. The suture material is looped over the clamp, and the short end of the stitch is pulled through the loop. The maneuver is repeated, but the loop is reversed, thereby creating a square knot. Transverse incisions may be closed with simple interrupted sutures through the fascia. The needle is reversed and is passed back through the skin, exiting on the same side as the initial needle bite. A straight cutting needle provides the best tool for placing a subcuticular stitch. The superficial muscle and uterine serosae are closed with running or running lock sutures of 0 Vicryl. After the serosa is closed, the bladder peritoneum is sutured to the uterus at the upper margin of the incision. This bladder laceration is closed with a 2-0 running chromic suture, which is placed through all layers of the bladder dome. The far-near fascial closure technique consists of an initial deep bite into the fascial margin, which protects against the suture cutting through the tissue. Typically, the suture material exceeds the tensile strength of the tissue, is tied too tightly, or is placed too close to the cut edge of the fascia. Closure of the burst abdomen is accomplished with #2 Prolene or #28 or stainless steel wire as a mass closure.
The peritoneum (parietal) supporting the cecum to the right abdominal gutter is cut (dashed line) antibiotics for sinus infection purchase 400 mg myambutol overnight delivery. The underlying psoas major muscle, common iliac vessels, and ureter are brought into clear view. The right common iliac vessels, the vena cava, and the ureter are brought into view. The uterine vessels are shown crossing the ureter at the level of the cardinal ligament. Note the right ovarian vessels cut and ligated but overlying the ureter on the right side. This view is oriented to allow observation of the field from above, looking caudally. The lateral peritoneal attachments of the sigmoid and descending colon are cut along the left gutter (dashed line in inset), permitting free mobilization of the large bowel. The left ovarian vessels, which overlie the ureter, have been removed in this drawing. The ovarian vessels (infundibulopelvic ligament) are not shown in this drawing. The ovarian vessels have been pulled laterally to separate them from the ureters and to better expose the ureters. The cardinal ligaments have been exposed by incising the posterior leaf of the broad ligament. Note the uterine vessels above and the vaginal vessels below as the ureters curve inward during their short journey through the cardinal ligaments. The infundibulopelvic ligament (ovarian vessels) has been retracted laterally and away from the ureters in this picture. In actual dissection, the ovarian vessels and the ureters cross over the common iliac vessels very close to one another. The dashed line shows how an incision will be made through the top of the ligament and extended to open the anterior and posterior leaves. The loose areolar tissues between the leaves have been dissected to expose the deeply situated left ureter. Tonsil clamps are placed on the uterine artery to divide it above the point where the ureter crosses under it. The uterine artery is a major branch of the anterior division of the hypogastric artery. The uterine artery in the vicinity of the junction of the cervix and uterine body splits into ascending and descending branches. The former is a coiled vessel that makes its way up the side of the uterus beneath the round ligament to the area between the junction of the tube, utero-ovarian ligament, and upper uterine corpus. Just before the uterine artery bifurcation, the vaginal artery may come off a common trunk, with the uterine artery. Alternatively, the vaginal artery may arise directly as a branch of the main hypogastric artery. Several sources of collateral circulation may be observed relative to the pelvic viscera. Although the hypogastric artery may be bilaterally ligated, blood flow to the pelvic organs continues via these collaterals. The vagina is a musculoepithelial tube extending from the level of the external genitals to the cervical portion of the uterus. It is a reproductive conduit in all respects, connecting the external environment to the internal genitalia. Anatomically, the vagina is anchored caudally and directly at the introitus by the levator ani muscles and bulbocavernosus muscles. Indirectly, other structures may contribute to the caudal vaginal support; these include the external sphincter ani, superficial transverse perineal muscles, and the perineal membrane. The anterior and posterior vaginal walls share fascial support in a manner analogous to that in unibody automobile construction with the bladder/urethra and rectum/anus. The vagina is intimately close to the bulb of the vestibule and clitoral apparatus. At the upper (cranial) end, the vagina shares support with the same structures that support the uterus. Between the two terminals, the vagina is relatively flexible and may be easily freed from surrounding fatty tissue and loose fascia. Anteriorly and posteriorly, the potential spaces are the vesicovaginal and rectovaginal, respectively. Laterally, on either side, the free space may be identified by cutting medially to the bulbocavernosus and levator ani muscles and developing the space along the outer wall of the vagina. The relationship of the lower ureters to the uterosacral ligaments and anterolateral vagina is important in that injuries to the ureters are most likely to occur in areas where there is proximity of structures such as these. Similarly, the cervix uteri and anterior fornix of the vagina are intimately close to the bladder base (trigone and interureteric ridge). The hypogastric plexus is anterior to the lower aorta and enters the presacral space from above over the retroperitoneal fat anterior to the left common iliac vein and middle sacral vessels and to the right of the inferior mesenteric vessels. As the plexus descends into the hollow of the sacrum, it typically splits into right and left divisions. The inferior hypogastric plexuses join other nerves to form the pelvic plexuses, which in turn are named for the organ with which they are associated. The hypogastric plexus is a conduit for autonomic nerves, as well as visceral pain fibers. Several of the large nerves of the pelvis and inferior extremity originate deep in the retroperitoneum of the lower abdomen and pelvis. The lumbar plexus is buried deeply beneath the substance of the psoas major muscle.
Activating hotspot mutations for Rac1 have been observed in 56% of melanomas (Hodis et al virus that shuts down computer buy genuine myambutol on-line. A handful of non-neural crestassociated neuronal proteins have been identified in melanoma cells (Namkoong et al. This finding is not surprising and implies that although oncogenes are important to drive the metastatic process to distant organs such as the brain, they may have a less important role in the outcome following the establishment of the lesion at the particular metastatic site. Therefore, other factors related with the "soil," either local (brain microenvironment) or systemic (host immune response), may be important. Nevertheless, presence of such mutations was more frequently associated with symptomatic brain metastases requiring active treatment (Koay et al. In addition, any histopathologic changes observed may actually reflect treatment effect. First, melanoma cells are frequently apposed to the abluminal surfaces of vessel walls, a phenomenon that has been previously termed angiotropism (Hung et al. Third, there is evidence of infiltration of adjacent glia by melanoma cells, either as single cells or as cell clusters. Fourth, pigmentation is present; this could either be attributed to deposition of hemosiderin secondary to chronic hemorrhage, or due to melanin that is either present within melanoma cells or "ingested" by tissue macrophages, termed melanophages. Abbreviations: tu, tumor; im, immune infiltrate; aHem, acute hemorrhage; cHem, chronic hemorrhage; gl, reactive glia; pig, pigment. Third, the clinical benefit of immunotherapies even in patients with active brain metastases, as will be discussed below (Margolin et al. In contrast, the extent of necrosis, melanin, and gliosis did not achieve any prognostic significance (Hamilton et al. Although the prognostic significance of intracranial hemorrhage quantified by nonhistopathologic methods, has been previously reported (Liew et al. Our group has also performed whole genome expression profiling of 29 melanoma specimens from the original 100-patient craniotomy cohort. Please note differential expression of various proteins by different cells within the melanoma brain metastatic lesions (tu, tumor; im, immune infiltrates; gl, reactive glia). Source: Immunoblot images were a courtesy of Drs Janiel Shields and Maria Sambade, University of North Carolina at Chapel Hill. These findings may revisit the prevailing clinical assumption that "peritumoral edema = adverse prognosis," and reconsider a prevailing clinical practice that any brain tumor with any degree of peritumoral brain edema must be treated with corticosteroids, an immunosuppressive strategy. Such intriguing results should obviously be confirmed in larger prospective studies. Reactive glia promotes tissue integrity, restricts inflammation, and, possibly, neuronal death (Yang et al. Nevertheless, the lack of association may be attributed to the crude histopathologic definition that was used to describe the response of the adjacent brain toward melanoma, namely the presence of reactive astrocytes with abundant eosinophilic cytoplasm and large displaced nucleus in the brain parenchyma near the tumor. Further in vitro studies using the melanomaastrocyte coculture model have further shown that glia may render melanoma cells less sensitive to systemic treatments. More specifically, coculture between immortalized astrocyte cell lines with melanoma cells revealed that astrocytes form multiple podia in direct contact with tumor cells. Furthermore, treatment of melanoma cells with chemotherapeutic agents attenuated apoptosis when melanoma cells were cocultured with astrocytes (Lin et al. Treatment of these shortterm cultures with astrocyte-conditioned medium obtained from immortalized human fetal astrocytes lead to significant upregulation of the Akt pathway and stimulated melanoma invasiveness compared with fibroblast conditioned medium (Niessner et al. The nature of paracrine factor(s) secreted by reactive glia that may influence tumor cell growth is currently under investigation (Valiente et al. Preclinical Animal Models to Study Melanoma Brain Metastases Most genetically engineered mouse melanoma models rarely develop spontaneous distant metastases. Admittedly, however, none of the genes that were disrupted in these two models appear to have a direct role in melanoma biology. Melanoma cells that were able to establish brain metastases following intracardiac or intracarotid injection were efficient in their ability to adhere to brain endothelial cells and proliferate in the presence of brain-conditioned medium (Cruz-Munoz et al. Although the immunohistochemical expression of most of these molecules was confirmed in tumor specimens from human craniotomies, the results from these studies should be interpreted with caution due to the inherent lack of a fully functioning host immune system. These models are immunocompetent and therefore overcome the challenges of interpretation of results from xenograft studies. Their weaknesses stem from the fact that these are essentially murine melanoma models; therefore, the interpretation of the findings for the human disease, including testing human, clinical-grade treatment, may not be possible. Humanized models of melanoma, which will be comprised of immune system reconstituted within immunodeficient mice. This mechanism may predominantly affect agents that are expected to have a direct antitumor effect, such as the small molecule inhibitors vemurafenib, dabrafenib, and trametinib. In addition, other mechanisms may account for the treatment benefit exerted by immunotherapies. It is also possible that the brain microenvironment may protect melanoma cells from cell death. Second, identification and targeting of other signaling pathways on which melanoma cells may depend for survival within the brain. Fourth, targeting the brain tumor microenvironment may maximize benefit from direct antitumor strategies. However, increasing evidence suggests that radiation therapy induces systemic effects beyond its ability to effectively control local disease. It is now established that radiation therapy requires functional immune system for maximum benefit (Lee et al.